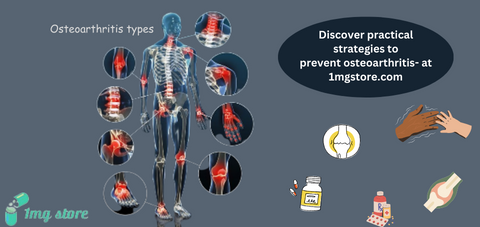
Osteoarthritis
- Generic: TriamcinoloneEquivalent Brand: Kenalog10 Injection$30.00
- Generic: Glucosamine SulphateEquivalent Brand: Cartigen30 Capsule/s$17.33
- Generic: TriamcinoloneEquivalent Brand: Kenalog30 Tablet/s$10.00
- Generic: TriamcinoloneEquivalent Brand: Kenalog30 Tablet/s$8.00Out of stock
Osteoarthritis (OA) is a degenerative joint disease characterized by the gradual breakdown of the cartilage that covers the ends of bones in the joints. It is the most common form of arthritis and can affect various joints, but it often occurs in the knees, hips, hands, and spine. Osteoarthritis typically develops slowly over time and is associated with aging, joint wear and tear, and certain risk factors.
Key Features of Osteoarthritis:
Cartilage Degeneration:
- Normal Joint Function: Healthy joints are cushioned by cartilage, which allows for smooth movement and absorbs shock during activities.
- Cartilage Breakdown: In osteoarthritis, the cartilage gradually breaks down, leading to friction between bones during movement.
Joint Pain and Stiffness:
- Pain: Osteoarthritis often presents with joint pain, especially during or after movement.
- Stiffness: Stiffness in the affected joints, particularly in the morning or after periods of inactivity, is common.
Joint Swelling:
- Inflammation: In some cases, inflammation may occur in the joint, leading to swelling and warmth.
Reduced Range of Motion:
- Limited Mobility: As osteoarthritis progresses, individuals may experience a reduction in the range of motion in the affected joint.
- Joint Instability:
- Weakness and Instability: Weakening of the muscles around the joint and changes in the joint structure can contribute to instability.
Risk Factors:
- Age: Osteoarthritis becomes more common with age, particularly in individuals over 50.
- Gender: Women are more prone to osteoarthritis, especially after menopause.
- Obesity: Excess weight increases the risk, as it places additional stress on weight-bearing joints.
- Joint Injuries: Previous joint injuries or trauma can contribute to the development of osteoarthritis.
- Genetics: A family history of osteoarthritis may increase the risk.
Diagnosis:
- Clinical Evaluation: Healthcare providers assess symptoms, medical history, and conduct a physical examination.
- Imaging Studies: X-rays, magnetic resonance imaging (MRI), or computed tomography (CT) scans may be used to visualize joint damage.
Treatment Options:
- Lifestyle Modifications: Weight management, exercise, and joint protection strategies are essential.
- Medications: Pain relievers, nonsteroidal anti-inflammatory drugs (NSAIDs), and in some cases, joint injections may be prescribed.
- Physical Therapy: Strengthening exercises and physical therapy can improve joint function and reduce pain.
- Surgical Interventions: In severe cases, joint replacement surgery may be considered.
Disease Management:
- Patient Education: Understanding the condition and adopting healthy lifestyle habits are crucial for long-term management.
- Regular Monitoring: Ongoing monitoring by healthcare professionals helps track disease progression and adjust treatment plans.
Research and Innovations:
- Advancements: Ongoing research aims to discover new treatment modalities, disease-modifying drugs, and interventions to improve the quality of life for individuals with osteoarthritis.
Conclusion:
Osteoarthritis is a common and progressive joint disease that significantly impacts the lives of affected individuals. While there is no cure, effective management strategies, including lifestyle modifications and various treatment options, can help alleviate symptoms and improve function. Continued research and a holistic approach to patient care contribute to enhancing the understanding and management of osteoarthritis. Early diagnosis and proactive management are key to maintaining joint health and optimizing the overall well-being of those living with osteoarthritis.