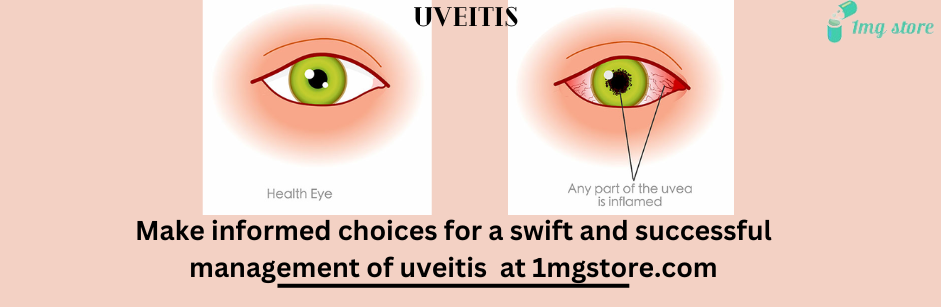
Uveitis
- Generic: CyclosporineEquivalent Brand: Neoral30 Capsule/s$17.50
- Generic: CyclopentolateEquivalent Brand: Cyclogyl1 Eye Drop$4.00
Understanding Inflammation of the Eye's Middle Layer
Uveitis refers to the inflammation of the uvea, the middle layer of the eye. The uvea consists of the iris, ciliary body, and choroid, and inflammation in this region can have significant implications for vision and overall eye health. Here's a comprehensive overview of uveitis, covering its types, causes, symptoms, diagnosis, treatment, and potential complications.
1. Types of Uveitis:
Anterior Uveitis (Iritis):
- Inflammation of the iris, the colored part of the eye.
Intermediate Uveitis (Cyclitis):
- Inflammation in the ciliary body, located between the iris and choroid.
Posterior Uveitis (Choroiditis):
- Affects the choroid, the layer at the back of the eye, and can involve the retina.
Panuveitis:
- Involves inflammation throughout the uvea.
2. Causes of Uveitis:
Autoimmune Disorders:
- Conditions like rheumatoid arthritis, lupus, or ankylosing spondylitis.
Infections:
- Bacterial, viral, or fungal infections affecting the eye.
Trauma:
- Eye injuries can lead to uveitis.
Inflammatory Diseases:
- Conditions such as inflammatory bowel disease or sarcoidosis.
Idiopathic:
- In some cases, the cause remains unknown.
3. Symptoms of Uveitis:
Eye Redness:
- Visible redness or bloodshot appearance.
Eye Pain:
- Often described as aching or throbbing.
Photophobia:
- Sensitivity to light.
Blurred Vision:
- Vision may become hazy or unclear.
Floaters:
- Perceived specks or particles in the field of vision.
Tearing:
- Excessive tearing unrelated to emotions.
4. Diagnosis:
Eye Examination:
- Detailed examination of the eye's structures.
Visual Acuity Test:
- Measures the clarity of vision.
Slit-Lamp Biomicroscopy:
- Magnified view of the eye's anterior segment.
Ophthalmoscopy:
- Examination of the retina and posterior segment.
Blood Tests:
- May be conducted to identify underlying causes.
5. Treatment Options:
Corticosteroids:
- Topical or systemic steroids to reduce inflammation.
Immunosuppressive Medications:
- Used in cases of autoimmune-related uveitis.
Antibiotics or Antivirals:
- If infection is the cause.
Pain Management:
- Analgesics for pain relief.
Dilation of Pupil:
- Eye drops to dilate the pupil, reducing discomfort.
6. Complications:
Glaucoma:
- Increased intraocular pressure.
Cataracts:
- Clouding of the eye's lens.
Retinal Detachment:
- Separation of the retina from its underlying layers.
Vision Loss:
- Severe cases may lead to permanent vision impairment.
7. Follow-Up and Monitoring:
Regular Eye Exams:
- Essential for monitoring progress and detecting complications.
Adjustment of Treatment:
- Treatment may be modified based on the response and recurrence of symptoms.
8. Conclusion:
Uveitis demands prompt diagnosis and appropriate management to prevent vision-threatening complications. Early recognition of symptoms, thorough examination, and adherence to treatment are vital for minimizing the impact of uveitis on eye health. Individuals experiencing eye redness, pain, or changes in vision should seek immediate medical attention for a comprehensive eye evaluation.