Rheumatic fever
-
Generic: Penicillin GEquivalent Brand: Pfizerpen60 Tablet/s$9.13
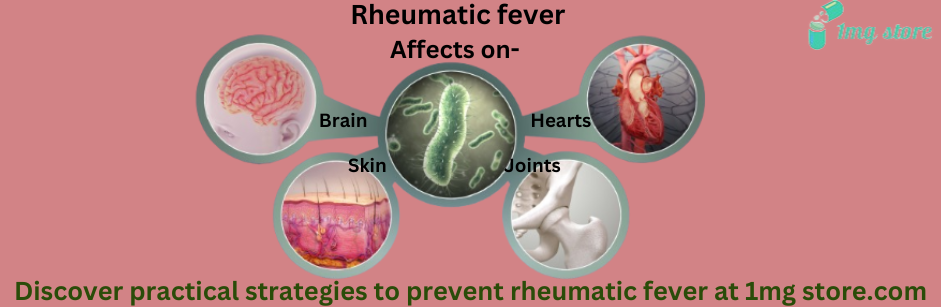
Rheumatic fever is a complex inflammatory disease that can develop as a complication of inadequately treated streptococcal throat infections, primarily caused by Group A Streptococcus bacteria. It primarily affects children and adolescents, and if left untreated, it can lead to severe and potentially life-threatening complications. This comprehensive overview will delve into the various aspects of rheumatic fever, including its causes, clinical manifestations, diagnosis, treatment, and preventive measures.
1. Introduction to Rheumatic Fever:
Rheumatic fever is an autoimmune inflammatory disease that primarily affects the joints, heart, skin, and nervous system. It is characterized by the development of inflammatory lesions, which are a result of the immune system's response to a preceding Group A Streptococcus (GAS) infection, typically a throat infection. The link between streptococcal infections and rheumatic fever was first established in the late 19th century, and despite advancements in medical science, it remains a significant health concern in some parts of the world.
2. Causes and Pathogenesis:
Rheumatic fever is triggered by an abnormal immune response to an untreated or inadequately treated streptococcal infection. The precise mechanisms that lead to the development of rheumatic fever are complex and involve both genetic and environmental factors. The following steps elucidate the pathogenesis of rheumatic fever:
a. Streptococcal Infection:
- Group A Streptococcus (GAS): Rheumatic fever is commonly associated with infections caused by GAS, particularly those affecting the throat, such as strep throat or tonsillitis.
b. Immune Response:
- Molecular Mimicry: The GAS bacteria contain antigens that structurally mimic proteins found in human tissues, especially in the heart, joints, and brain.
- Autoimmune Response: Following a streptococcal infection, the immune system may mistakenly target its own tissues due to the resemblance between bacterial antigens and human proteins.
c. Inflammatory Lesions:
- Formation of Nodules: Inflammatory lesions, known as Aschoff nodules, may develop in various organs, particularly the heart.
- Immune Complexes: The immune system forms immune complexes, leading to inflammation in affected tissues.
3. Clinical Manifestations:
The clinical presentation of rheumatic fever is diverse, and symptoms may vary widely among affected individuals. The disease typically occurs 2-4 weeks after a streptococcal infection. The major clinical manifestations include:
a. Rheumatic Arthritis:
- Joint Involvement: Joints, especially larger ones like the knees, ankles, elbows, and wrists, may become inflamed, causing pain, swelling, and stiffness.
- Migratory Nature: Joint pain tends to migrate from one joint to another.
b. Carditis:
- Inflammation of the Heart: Carditis affects the heart and can lead to complications such as valvular damage.
- Murmurs: Heart murmurs may be heard on auscultation.
c. Subcutaneous Nodules:
- Painless Nodules: Subcutaneous nodules may develop under the skin, typically over bony prominences.
- Palpable and Mobile: These nodules are usually firm, painless, and mobile when palpated.
d. Erythema Marginatum:
- Skin Rash: Erythema marginatum is a rash characterized by pink, non-pruritic, and serpentine lesions with a clear center.
- Trunk and Proximal Extremities: The rash typically appears on the trunk and proximal extremities.
e. Sydenham's Chorea:
- Involuntary Movements: Sydenham's chorea is a neurological manifestation characterized by involuntary, purposeless movements.
- Facial Grimacing: Facial grimacing, impaired handwriting, and muscle weakness may be observed.
4. Diagnosis:
Diagnosing rheumatic fever involves a comprehensive approach, considering clinical criteria, laboratory tests, and evidence of a recent streptococcal infection. The Jones Criteria, established by the American Heart Association, are commonly used for diagnosis:
a. Clinical Criteria:
- Arthritis: Evidence of migratory polyarthritis.
- Carditis: Signs of inflammation involving the heart, such as murmurs.
- Subcutaneous Nodules: Presence of subcutaneous nodules.
- Erythema Marginatum: Characteristic skin rash.
- Sydenham's Chorea: Neurological manifestations.
b. Laboratory Tests:
- Elevated Acute Phase Reactants: Increased levels of acute-phase reactants, such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP).
- Positive Streptococcal Tests: Evidence of a recent streptococcal infection, including positive throat cultures or rapid streptococcal antigen tests.
c. Electrocardiogram (ECG) and Echocardiography:
- Cardiac Assessment: ECG and echocardiography are essential for evaluating cardiac involvement and identifying valvular abnormalities.