High Triglycerides
- Generic: GemfibrozilEquivalent Brand: Lopid30 Tablet/s$15.50
$96.8 - Generic: AtorvastatinEquivalent Brand: Lipitor30 Tablet/s$9.00
- Generic: FenofibrateEquivalent Brand: Fenoglide30 Tablet/s$18.00
- Generic: AtorvastatinEquivalent Brand: Lipitor30 Tablet/s$4.32
$127.31
Understanding High Triglycerides: Causes, Risks, and Management
High triglycerides, a type of fat (lipid) found in the blood, are a significant health concern affecting millions of individuals worldwide. Elevated triglyceride levels, known as hypertriglyceridemia, can increase the risk of cardiovascular disease and other health complications. In this comprehensive guide, we will explore the causes, risks, and management strategies for high triglycerides, empowering you with valuable information to take proactive steps toward better health.
What Are Triglycerides?
Triglycerides are a type of lipid found in the bloodstream and stored in fat cells. They are derived from the fats we eat in our diet as well as those produced by the liver. Triglycerides serve as a source of energy for the body's cells, but elevated levels can lead to health problems. When you consume more calories than your body needs, the excess calories are converted into triglycerides and stored in fat cells for later use.
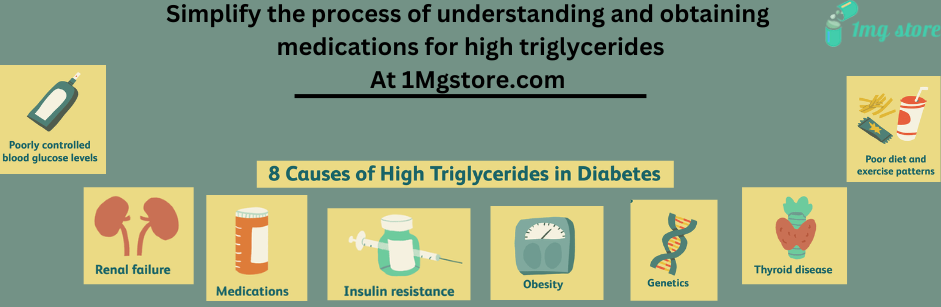
Causes of High Triglycerides:
Several factors can contribute to high triglyceride levels, including:
- Unhealthy Diet: Diets high in sugar, refined carbohydrates, and unhealthy fats (such as saturated and trans fats) can lead to elevated triglyceride levels. Consuming sugary beverages, sweets, processed foods, and fried foods can contribute to the accumulation of triglycerides in the bloodstream.
- Excess Alcohol Consumption: Alcohol is metabolized by the liver, and excessive alcohol consumption can lead to an increase in triglyceride production. Chronic alcohol consumption can also impair liver function, leading to higher triglyceride levels.
- Obesity and Overweight: Being overweight or obese is strongly associated with elevated triglyceride levels. Excess body fat, particularly abdominal fat, can lead to insulin resistance, metabolic abnormalities, and increased triglyceride production.
- Physical Inactivity: Lack of regular physical activity can contribute to higher triglyceride levels. Exercise helps lower triglycerides by increasing the breakdown of fats for energy and improving insulin sensitivity.
- Genetics: Genetic factors can influence triglyceride levels. Some individuals may have a genetic predisposition to higher triglyceride levels, even with a healthy lifestyle.
Certain Medical Conditions: Underlying medical conditions such as diabetes, hypothyroidism, kidney disease, and liver disease can lead to elevated triglyceride levels. Hormonal imbalances and medications (such as corticosteroids, estrogen, and certain antipsychotic drugs) can also affect triglyceride metabolism.
Risks Associated with High Triglycerides:
High triglyceride levels are a significant risk factor for various health complications, including:
- Cardiovascular Disease: Elevated triglyceride levels are associated with an increased risk of coronary artery disease, heart attack, and stroke. Triglycerides contribute to the formation of plaque in the arteries (atherosclerosis), leading to narrowed or blocked blood vessels and reduced blood flow to the heart and brain.
- Pancreatitis: Extremely high triglyceride levels (typically above 500 mg/dL) can lead to acute pancreatitis, a serious inflammation of the pancreas. Pancreatitis can cause severe abdominal pain, nausea, vomiting, and in severe cases, organ failure and death.
- Metabolic Syndrome: High triglyceride levels are often part of a cluster of risk factors known as metabolic syndrome, which also includes abdominal obesity, high blood pressure, and insulin resistance. Metabolic syndrome significantly increases the risk of heart disease, stroke, and type 2 diabetes.
- Type 2 Diabetes: Elevated triglyceride levels are commonly observed in individuals with type 2 diabetes. Insulin resistance, a hallmark of type 2 diabetes, leads to increased triglyceride production by the liver and decreased clearance of triglycerides from the bloodstream.
Screening and Diagnosis:
- Triglyceride levels can be measured through a simple blood test called a lipid profile or lipid panel. This test typically measures total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides. Fasting for 8-12 hours before the test is often required to obtain accurate results.
- The American Heart Association (AHA) recommends regular lipid screening for adults starting at age 20 and repeating it every four to six years if the results are within the normal range. However, individuals with known risk factors for cardiovascular disease or those with a family history of high triglycerides may require more frequent monitoring.
Lifestyle Modifications for Managing High Triglycerides:
Making lifestyle changes is essential for managing high triglyceride levels and reducing the risk of cardiovascular complications. Here are some effective strategies:
- Follow a Healthy Diet: Adopt a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats (such as those found in fish, nuts, and avocados). Limit the intake of sugary beverages, sweets, refined carbohydrates, and saturated fats.
- Limit Alcohol Consumption: If you drink alcohol, do so in moderation. Limit alcohol intake to no more than one drink per day for women and no more than two drinks per day for men. Avoid binge drinking and excessive alcohol consumption, as it can significantly raise triglyceride levels.
- Maintain a Healthy Weight: Achieve and maintain a healthy weight through a combination of balanced diet and regular physical activity. Aim for a body mass index (BMI) within the healthy range (18.5 to 24.9 kg/m²) and focus on reducing abdominal fat, as excess abdominal fat is particularly associated with elevated triglyceride levels.
- Engage in Regular Exercise: Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week, along with muscle-strengthening activities on two or more days per week. Exercise helps lower triglycerides, improve insulin sensitivity, and promote overall cardiovascular health.
- Quit Smoking: If you smoke, quit smoking as soon as possible. Smoking damages blood vessels, increases inflammation, and worsens lipid profiles, including triglyceride levels. Quitting smoking is one of the most significant steps you can take to improve your cardiovascular health.
- Manage Stress: Chronic stress can contribute to unhealthy lifestyle behaviors, such as overeating, poor dietary choices, and lack of exercise, which can exacerbate high triglyceride levels. Practice stress-reducing techniques such as mindfulness, meditation, deep breathing exercises, and engaging in hobbies or activities you enjoy.
Medications for High Triglycerides:
In some cases, lifestyle modifications alone may not be sufficient to lower triglyceride levels, particularly if they are extremely elevated or if there are underlying medical conditions. In such cases, medications may be prescribed to help lower triglycerides. Commonly used medications include:
- Statins: Statin medications are primarily used to lower LDL cholesterol levels but can also modestly reduce triglyceride levels. They work by inhibiting an enzyme involved in cholesterol synthesis in the liver.
- Fibrates: Fibrate medications, such as fenofibrate and gemfibrozil, are specifically designed to lower triglyceride levels and raise HDL cholesterol levels. They work by activating a protein that helps break down triglycerides in the blood.
- Omega-3 Fatty Acids: Prescription-strength omega-3 fatty acid supplements, such as prescription fish oil (icosapent ethyl), can help lower triglyceride levels, particularly in individuals with very high triglycerides (>500 mg/dL).
- Niacin (Nicotinic Acid): Niacin is a B vitamin that can help lower triglycerides and raise HDL cholesterol levels. However, niacin is associated with side effects such as flushing, itching, and liver toxicity, so it is typically used with caution and under medical supervision.
- Combination Therapies: In some cases, a combination of medications may be prescribed to achieve optimal lipid control. For example, a statin may be combined with a fibrate or omega-3 fatty acid supplement to target both LDL cholesterol and triglyceride levels.
Conclusion:
High triglyceride levels are a significant risk factor for cardiovascular disease and other health complications. By understanding the causes, risks, and management strategies for high triglycerides, you can take proactive steps to improve your lipid profile and overall health. Making lifestyle changes such as following a healthy diet, engaging in regular exercise, maintaining a healthy weight, limiting alcohol consumption, and managing stress can help lower triglyceride levels and reduce cardiovascular risk. In some cases, medications may be necessary to achieve optimal lipid control, particularly if lifestyle modifications alone are insufficient. Consult with your healthcare provider to develop a personalized treatment plan tailored to your individual needs and health goals. By taking control of your triglyceride levels, you can reduce your risk of heart disease and enjoy a healthier, more active life.