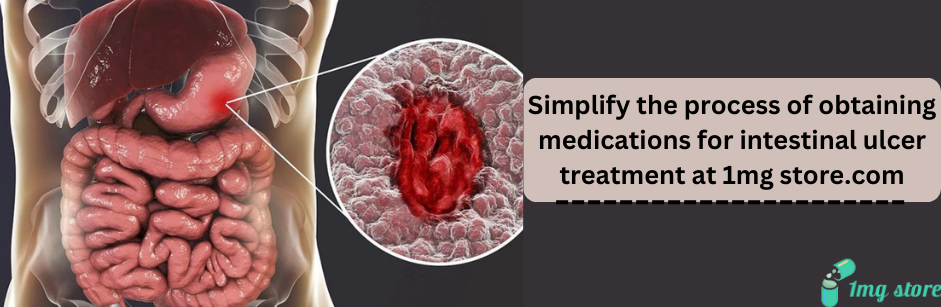
Intestinal Ulcers
Intestinal ulcers, also known as peptic ulcers, are sores or lesions that develop in the lining of the small intestine or other parts of the gastrointestinal tract. Similar to stomach ulcers, intestinal ulcers can cause various symptoms and complications. Here's an in-depth overview of intestinal ulcers, covering their causes, symptoms, diagnosis, and treatment:
1. Causes of Intestinal Ulcers:
a. Helicobacter pylori (H. pylori) Infection:
- A bacterial infection that can weaken the protective mucous layer of the intestines, leading to ulcer formation.
b. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
- Long-term use of NSAIDs, such as aspirin or ibuprofen, can irritate the intestinal lining and contribute to ulcer development.
c. Excessive Acid Production:
- Conditions that increase stomach acid production, such as Zollinger-Ellison syndrome.
d. Smoking and Alcohol:
- Lifestyle factors, including smoking and excessive alcohol consumption, may increase the risk of intestinal ulcers.
e. Stress:
- While stress alone does not cause ulcers, it may exacerbate existing conditions.
2. Symptoms of Intestinal Ulcers:
a. Abdominal Pain:
- Burning or gnawing pain in the mid to lower abdomen, often relieved by eating or taking antacids.
b. Indigestion:
- Bloating, belching, and a feeling of fullness.
c. Nausea and Vomiting:
- Queasiness, nausea, and vomiting.
d. Changes in Appetite:
- Loss of appetite and unintentional weight loss.
e. Dark Stools:
- Blood in the stool may cause it to appear dark or tarry.
f. Fatigue:
- Anemia resulting from slow, chronic bleeding.
3. Diagnosis of Intestinal Ulcers:
a. Endoscopy:
- A flexible tube with a camera is used to examine the intestines, allowing for the identification of ulcers.
b. Upper GI Series:
- X-ray imaging with contrast material to visualize the upper gastrointestinal tract.
c. Blood and Stool Tests:
- Testing for H. pylori infection or signs of gastrointestinal bleeding.
4. Treatment of Intestinal Ulcers:
a. Medications:
- Proton Pump Inhibitors (PPIs): Reduce stomach acid production.
- H2 Blockers: Decrease the amount of acid produced by the stomach.
- Antibiotics: If H. pylori is present, a course of antibiotics may be prescribed.
b. Antacids:
- Over-the-counter antacids can provide relief from symptoms.
c. Lifestyle Modifications:
- Quitting smoking and moderating alcohol intake.
d. Diet Changes:
- Avoiding spicy foods, caffeine, and other irritants.
5. Complications and Monitoring:
a. Bleeding Ulcers:
- Severe cases may lead to gastrointestinal bleeding and require emergency medical attention.
b. Perforation or Obstruction:
- Rarely, ulcers may cause perforation or blockage of the intestines, necessitating surgery.
c. Regular Follow-Up:
- Monitoring ulcer healing through follow-up endoscopies or imaging studies.
6. Importance of Lifestyle Changes:
a. Dietary Habits:
- Adopting a balanced diet rich in fruits, vegetables, and fiber.
b. Stress Management:
- Incorporating stress-reducing techniques into daily life.
7. When to Seek Medical Attention:
Prompt medical attention is necessary if:
- Symptoms persist or worsen.
- There is significant weight loss.
- Signs of bleeding, such as dark stools or vomiting blood, are present.
8. Conclusion:
Intestinal ulcers can be effectively managed with a combination of medications, lifestyle modifications, and, in some cases, antibiotics. Early detection and appropriate treatment are crucial to prevent complications and promote healing. Individuals experiencing symptoms of intestinal ulcers should seek medical evaluation for an accurate diagnosis and an effective treatment plan. Regular follow-up with healthcare professionals is essential to monitor progress and adjust the treatment regimen as needed.