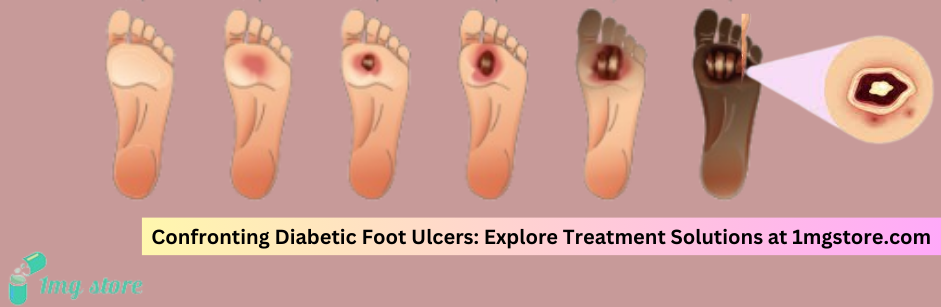
Diabetic Foot Ulcers
- Generic: Epidermal Growth FactorEquivalent Brand: Regen-D Gel1 Gel$40.33
Diabetic foot ulcers are a common complication of diabetes and a serious medical condition. These ulcers are open sores or wounds that typically develop on the feet of individuals with diabetes. Diabetes can lead to poor circulation and nerve damage, making the feet vulnerable to injuries that may go unnoticed due to reduced sensation. Here's an overview of diabetic foot ulcers:
Causes:
- Peripheral Neuropathy: Nerve damage, known as peripheral neuropathy, reduces sensation in the feet, making it difficult to detect injuries or pressure points.
- Poor Circulation: Diabetes can lead to blood vessel damage, reducing blood flow to the feet, impairing the body's ability to heal and fight infections.
- Foot Deformities: Conditions like Charcot foot, where the bones weaken and collapse, can contribute to the development of ulcers.
- Infections: Bacterial or fungal infections can complicate and delay the healing of wounds.
Symptoms:
- Open Sores or Wounds: Persistent wounds or sores on the feet that may be slow to heal.
- Redness and Swelling: The affected area may show signs of inflammation.
- Warmth: Increased warmth around the ulcer may indicate infection.
- Pain or Discomfort: Some individuals may experience pain, while others with neuropathy may not feel pain despite the severity of the ulcer.
Complications:
- Infection: Diabetic foot ulcers are prone to infections, which can spread to the surrounding tissues and bones.
- Cellulitis: Bacterial infection of the skin and underlying tissues.
- Osteomyelitis: Infection of the bone, which can lead to serious complications.
- Gangrene: Death of body tissue due to a lack of blood supply.
Prevention:
- Regular Foot Inspection: Check feet daily for cuts, blisters, or any abnormalities.
- Proper Foot Care: Keep feet clean, moisturized, and nails trimmed. Avoid going barefoot.
- Control Blood Sugar Levels: Maintain optimal blood glucose levels to promote healing.
- Choose Proper Footwear: Wear comfortable, well-fitted shoes to prevent pressure points and injuries.
- Regular Medical Check-ups: Regular foot examinations by healthcare professionals for early detection of potential issues.
Treatment:
- Wound Care: Cleaning and dressing the ulcer to promote healing.
- Offloading: Using devices like special shoes or casts to relieve pressure on the affected area.
- Infection Management: Antibiotics may be prescribed for infected ulcers.
- Debridement: Removal of dead or infected tissue to facilitate healing.
- Revascularization: In cases of poor circulation, procedures to improve blood flow may be considered.
Multidisciplinary Approach: The management of diabetic foot ulcers often involves a multidisciplinary team, including podiatrists, endocrinologists, vascular surgeons, and infectious disease specialists. Prevention, early detection, and prompt treatment are essential in minimizing complications and improving outcomes for individuals with diabetic foot ulcers.